The knee joint is formed by a mobile “tandem” of tibia and femur.The patella prevents its lateral displacement and an elastic layer of durable cartilage tissue ensures easy sliding movement.
The thickness of the "healthy" cartilage covering the articular surfaces of the bones of the knee joint is 5-6 mm.
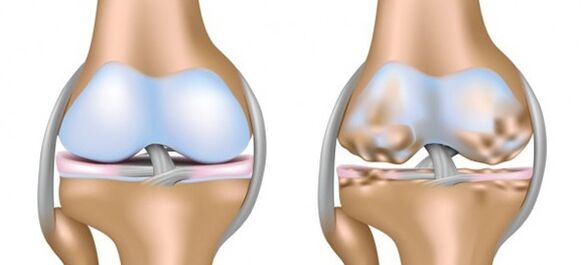
This is enough to soften the mechanical friction of the bones and absorb the "impact" load.A disease that leads to the destruction of the natural shock-absorbing tissue and deformation of the joint, gonarthrosis or osteoarthritis of the knee joint, has unpleasant symptoms and its treatment is often made difficult by the implementation of a compensatory mechanism of the bone structures.
What triggers the disease?
There is an opinion that knee gonarthrosis is a consequence of "salt deposition".However, calcification or deposition of calcium salts in the ligamentous apparatus of the knee does not have an independent meaning and is more of a consequence than a cause.
What is gonarthrosis and how to treat it?
In reality, the “starting point” should be considered the alteration of the blood supply to the small bone vessels and its consequence: the difficulty in the trophism of the cartilaginous tissue and its exhaustion.This is followed by deformation of the hyaline cartilage.The latter exfoliates and becomes covered with multidirectional cracks.The synovial fluid becomes more viscous and loses its properties as a natural "moisturizer" of the cartilage tissue.
The complete disappearance of the drying “buffer” could be considered the end of the pathological process.
However, underlying bones that have lost their cartilaginous "covering" compensate for the loss by growing along the periphery and covering themselves with "spikes" - bone growths.In this case, the knee joint is deformed and the legs acquire an X or O shape, which is why this pathology is also called deforming osteoarthritis of the knee joint (hereinafter referred to as DOA).
What are the causes of osteoarthritis of the knee joint?
- Aging of the body and the consequent “wear and tear” of the joints;
- Excess body weight;
- Extreme loads on the knee joint (in athletes);
- Knee injury, fracture of one of his bones;
- Removal of the meniscus;
- Untreated arthritis, rheumatism;
- Abnormal location of the bony components of the joint;
- “Failure” in the endocrine system and hormonal disharmony, metabolic imbalance.
Osteoarthritis is often confused with various arthritis.
However, the difference between arthritis and osteoarthritis of the knee joint is that the former is usually the result of the invasion of the body by various pathogens, which "cause" inflammatory diseases of the entire body.
Sometimes signs of arthritis (inflammation and swelling of the joint, swelling, pain that is worse at night) are the result of the immune system "unfolding" an active defense against the body's own cells.
Osteoarthritis, being an exclusively local disease, often becomes a logical continuation of arthritis or a consequence of the gradual "wear" of the joint.
Primary and secondary gonarthrosis.
In orthopedics and traumatology, types of osteoarthritis of the knee joint are usually distinguished based on the reasons that led to degenerative changes in the articular cartilage.
- Primary or age-related gonarthrosisThe knee joint often interrupts the course of relatively painless old age due to physical "wear" of the cartilaginous tissue.A little more often, compared to men, women who have passed the 40-year mark face this form of the disease.The earlier development of primary gonarthrosis threatens athletes and those who carry extra kilos;
- secondary gonarthrosis– a logical continuation of a previous injury or consequence of untimely treatment of inflammatory diseases, develops at any age.

Where is the disease hiding?
Gonarthrosis, which develops gradually, is located in the inner part of the knee joint.However, the disease can “lurk” between the kneecap and the surface of the femur.
- Left-sided gonarthrosis often affects athletes and overweight people;
- People whose professional or sports activities involve excessive dynamic or static loads on the right leg are more susceptible to degenerative changes in the cartilaginous layer of the right knee joint;
- Bilateral gonarthrosis is usually age-related.Regardless of the reasons, uncontrolled destruction of both knee joints in most cases leads to disability.
Oh, it hurts!
Signs of gonarthrosis of the knee joint at the beginning of the disease are rather vague, and not many people will rush to visit a rheumatologist or arthrologist if they feel pain in the knee after a long walk.
After all, a short rest and relaxation relieves unpleasant symptoms in a slightly "crunchy" knee, giving a dubious feeling of physical well-being.
In fact, the “vague” symptoms of the early stages of degenerative diseases of the musculoskeletal system make their timely detection and treatment extremely difficult.Gonarthrosis deformans is no exception.
- Stage 1 gonarthrosis, which is manifested only by slight discomfort caused by fatigue of the limb, is extremely difficult to recognize on one's own.A timely impetus to visit a doctor is often given by a dull pain in the knee and the "crunch" of rough cartilage sticking together;
- Second-degree gonarthrosis paves the way for deformation of the knee joint and makes it difficult to move in the morning, causing the need to "diverge".Severe, prolonged pain occurs after standing or sitting for a long time.Moderately limited knee mobility is accompanied by a cracking sound;
- The maximum signs of osteoarthritis of the knee joint appear in the third stage of the disease.A swollen knee, the local temperature of which increases, often hurts at rest.
The movement of the joint is blocked by acute pain caused by the "joint mouse" - fragments of broken bone growths.
A deformed joint loses stability and is difficult to move.Advanced disease at this stage requires prosthetics.
Can knee osteoarthritis be cured?
The well-known statement “Rest is not an end in itself, but a means to an end” is directly related to those facing the initial manifestations of the disease.Rest ensures maximum unloading of the knee joint during an exacerbation.For the same purpose, the use of individual orthopedic insoles is recommended.
The use of individual orthopedic insoles will ensure maximum relief of the knee joint.
A kind of insurance against the disease, or rather against its exacerbation, will be special orthoses that support the stability of the "loose" knee joint in athletes.
A cane will help older people "unload" their joints while walking.But the listed measures are more likely to prevent osteoarthritis of the knee joints.If such a "vaccine" did not help and worsened gonarthrosis manifests itself with inflammation and pain, you should hurry to consult an orthopedist or arthrologist.
How to treat gonarthrosis?
- Stage 1.Stop inflammation and the pain that accompanies it.Non-steroidal anti-inflammatory drugs used orally, intramuscularly or intravenously are those that best solve the "acute" problem.NSAIDs "sealed" in rectal suppositories will have a long effect.
The use of corticosteroids is also justified: they are "administered" directly into the diseased joint.
Topical use of ointments or gels with an active anti-inflammatory component will help enhance the anti-inflammatory effect of NSAIDs used internally.The latter help to quickly relieve swelling.

Medications that reduce vascular muscle tone are often prescribed along with NSAIDs.This improves periarticular blood flow.
What to do with osteoarthritis of the knee joint, for example, in patients suffering from gastrointestinal diseases for whom it is dangerous to take NSAIDs and pain relievers?
Oxygen therapy would be a good alternative.
- Stage 2.“Nourishes” dry cartilage with substances that stimulate collagen synthesis.Chondroprotectors intended for this purpose act slowly, but their prolonged use favors the synthesis of the natural components of the cartilage matrix.The greatest effect is achieved through intra-articular administration of drugs.
- Stage 3.We soften the “roughness” of the cartilage and reduce its friction by introducing hyaluronic acid.
- Stage 4.We improve blood supply and joint trophism through physiotherapy.To do this, it is recommended to combine business with pleasure and undergo sanatorium-resort treatment.
- Stage 5.We resort to non-traditional treatment methods: acupuncture and hirudotherapy, apitherapy.An innovation in the treatment of DOA of the knee joint is the intra-articular administration of Orthokine, a serum obtained from the patient's blood proteins.


What are the correct exercises to do?
Physiotherapy will help stop the progressive destruction of joint elements.Its main objectives:
- improve blood flow to the joint and activate the trophism of all its components;
- increased knee mobility;
- raising the tone of all the muscles of the human body.
It is recommended that physical therapy sessions, at least initially, be conducted under the supervision of a physical therapy instructor.An experienced trainer will select exercises that correspond to the level of mobility of the joint, excluding high-amplitude exercises and exercises with excessive axial loading, all of which can damage the soft tissues of the joint and worsen the patient's condition.
Recipes from the green pharmacy: there are options!
Provides gonarthrosis and treatment with traditional methods:
- Option 1.Grind 120 g of garlic, 250 g of celery root and 3 lemons in a meat grinder.Place the mixture in a 3 liter jug and fill to the top with boiling water.After keeping the composition overnight in a warm place, wrap the bottle well, start taking it in the morning, consuming 70 grams of the medicine each morning.Gradually increase intake up to 3 times;
- Option 2.Treat the sore joint with a mixture of 1 tbsp.l.honey and 3 tbsp.l.apple cider vinegarPlace a leaf of fresh cabbage on top (beat it lightly with a knife) or burdock (light side facing the joint).Wrap your leg with cellophane film and a soft scarf.Do it at night, up to 30 procedures.

Unavoidable decision
Often, severe pain and joint dysfunction threatens disability.
Then, middle-aged patients, as well as young people diagnosed with osteoarthritis of the knee joint, require surgery.
The most common procedure is endoprostheses.The duration of such an operation is no more than an hour and its effect is painless functioning of the "restored" limb for at least 20 years.Over time, the “loose” prosthesis will need to be replaced.






















